Microglia in Alzheimer’s research have emerged as a crucial focus in understanding the complexities of Alzheimer’s disease. These specialized microglial cells act as the brain’s immune system, continuously surveilling the central nervous system for signs of damage or disease. In the pursuit of breakthroughs, neuroscientist Beth Stevens has highlighted the pivotal role of these cells in synaptic pruning—the process of eliminating excess connections in neuronal networks. However, when this process goes awry, it can contribute to the progression of neurodegenerative disorders like Alzheimer’s, underscoring the need for targeted research. Stevens’ work, supported by rigorous Alzheimer’s disease research, promises new avenues for therapies that could potentially transform the lives of millions affected by cognitive decline.
Exploring the role of glial cells in dementia research reveals a promising avenue for therapeutic intervention against cognitive decline. These brain-resident immune cells, known for their function in maintaining homeostasis, are gaining recognition for their involvement in sculpting neural connections through a process called synaptic elimination. The groundbreaking findings from researchers like Beth Stevens suggest that abnormal activity of these cells could play a pivotal role in the development of conditions such as Alzheimer’s and other neurodegenerative diseases. By examining the intricacies of the brain’s immune system, scientists are opening new frontiers in understanding and treating these devastating disorders. This fresh perspective on neural health articulates the importance of examining cellular interactions within the brain’s architecture to unveil paths to potential cures.
Understanding the Role of Microglial Cells in Alzheimer’s Disease
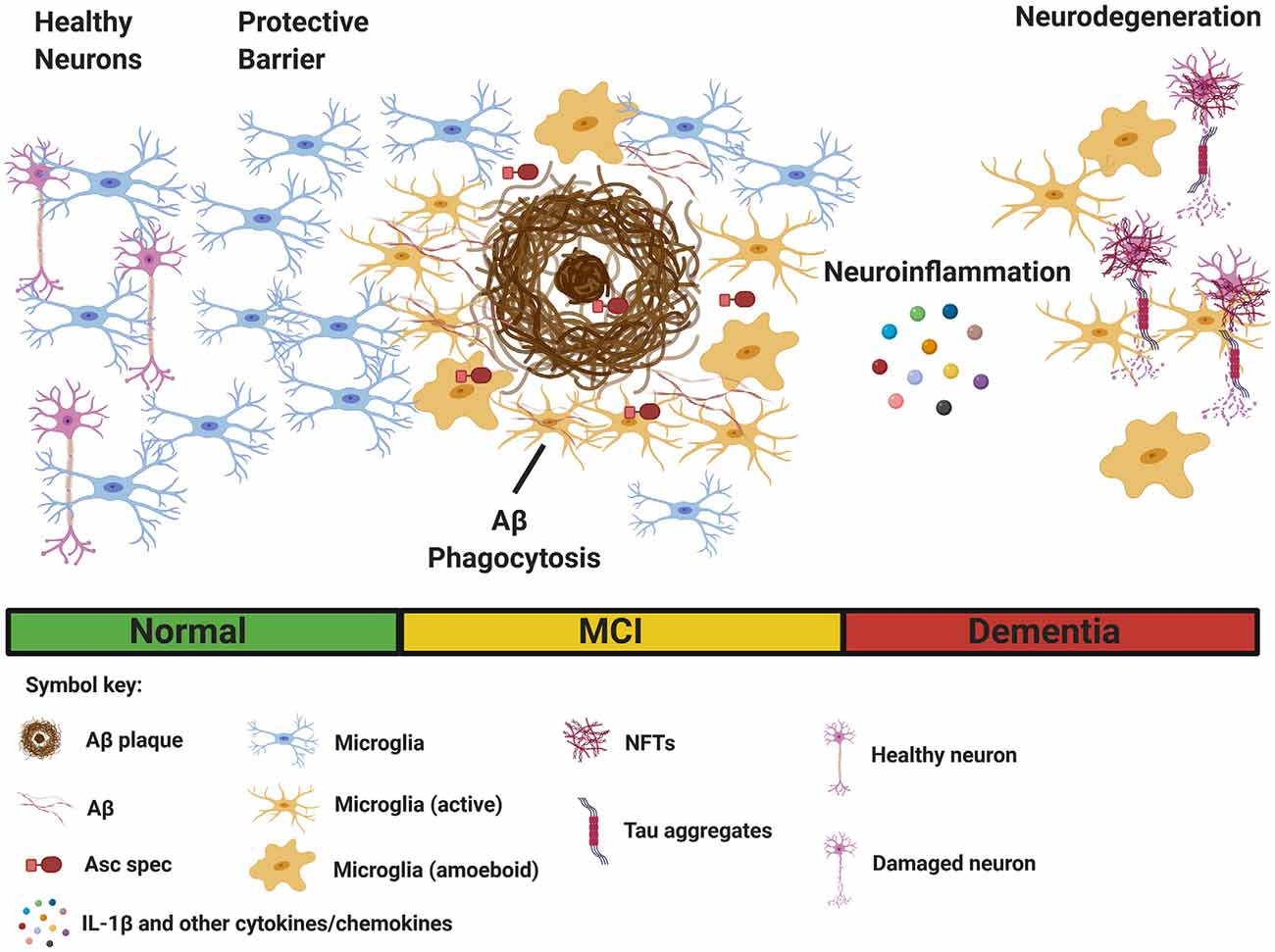
Microglial cells, often referred to as the brain’s immune system, play a pivotal role in maintaining neuronal health and functionality. These specialized cells are responsible for surveying the central nervous system for signs of disease or injury, effectively acting as guardians of our brain environment. In the context of Alzheimer’s disease, research has uncovered that dysregulated microglial activity can lead to impaired synaptic pruning — the process whereby excess synapses, which are often involved in the transmission of signals between neurons, are eliminated. This aberrant pruning contributes to the neurodegenerative nature of Alzheimer’s, where synaptic loss can result in cognitive decline and memory issues. Understanding how microglial cells interact with neurons is essential for developing strategies to treat, or even prevent, Alzheimer’s disease.
Recent studies suggest that an overactive or malfunctioning microglial response can exacerbate neuroinflammation, a hallmark of Alzheimer’s disease. This vicious cycle not only leads to increased synaptic damage but also impacts other brain functions, perpetuating a decline into further neurodegeneration. By targeting microglial pathways, researchers aim to develop novel therapies that can modulate these immune responses, potentially restoring the balance necessary for healthy brain function. The ongoing research into microglia in Alzheimer’s research pulsates with optimism as it lays a foundation that could revolutionize treatment approaches for millions suffering from this devastating condition.
The Importance of Synaptic Pruning in Neurodevelopment
Synaptic pruning is a critical process in the maturation of brain circuits, where microglial cells play a key role in selecting and eliminating unnecessary synapses. During early development, the brain produces an overabundance of synapses — more than will ultimately be retained. This is where microglial cells come into play, using a series of signals to determine which synapses should be preserved and which should be trimmed away. This carefully orchestrated event is essential for optimizing neuronal connections and ensuring efficient communication within the brain. Disruption in this process can lead to various neurodevelopmental disorders, highlighting the integral role of microglia in both healthy development and the onset of diseases.
In the context of neurodegenerative diseases like Alzheimer’s, improper synaptic pruning can result in the loss of critical neural networks, exacerbating cognitive decline and functional impairment. The research by Beth Stevens has illuminated how aberrant microglial activity can lead to improper synapse elimination, leading to the grey matter atrophy typical in Alzheimer’s patients. Hence, targeting the mechanisms of synaptic pruning can aid in restoring balance and functional connectivity in the aging brain. This focus on the role of microglia and their influence on synaptic health paves the way for innovative therapeutic strategies that could alleviate or even reverse some aspects of neurodegenerative disorders.
Microglial Cells as a Biomarker for Alzheimer’s Disease
Recent advancements in Alzheimer’s disease research have highlighted the potential of microglial cells as biomarkers for early detection and progression monitoring of the disease. As these immune cells respond to neurodegenerative changes in the brain, their activation state and morphology can provide insight into the neuroinflammatory processes that occur in Alzheimer’s. By profiling microglial activity, researchers can develop indicators that help in diagnosing Alzheimer’s during its early stages when treatment may be more effective. This paradigm shift may significantly enhance our approach to Alzheimer’s disease, moving us towards a more proactive rather than reactive stance in managing this complex condition.
Furthermore, leveraging the characteristics of microglial cells could lead to the development of personalized medicine strategies tailored to individual patient profiles. The variability in microglial response can offer valuable information about a patient’s specific disease pathology, assisting clinicians in making informed decisions regarding treatment options. Additionally, understanding the nuances of microglial function could inspire novel therapeutic avenues that target neuroinflammation, ultimately aiming to slow down disease progression and improve the quality of life for those affected by Alzheimer’s and similar neurodegenerative disorders.
The Evolution of Neuroinflammation Research
The field of neuroinflammation research has undergone a significant evolution, transforming our understanding of the brain’s immune responses in health and disease. Years ago, neuroinflammation was often overlooked in favor of focusing on neuronal pathology when addressing neurodegenerative diseases like Alzheimer’s. However, as studies on microglial cells have advanced, it has become clear that neuroinflammation plays a critical role in neuronal health and the progression of neurodegenerative diseases. The recognition of microglia as key players in this inflammation has opened a new frontier in neuroscience, emphasizing the need for interdisciplinary approaches that incorporate immunology within studies of neurodegeneration.
Innovations in imaging techniques and molecular biology have allowed researchers to visualize microglial activation in real-time, shedding light on their role in various neurodegenerative conditions. These advancements have enabled scientists to investigate how microglial dysfunction may lead to chronic inflammation, thereby accelerating neuronal damage and accelerating diseases like Alzheimer’s. As a result, ongoing research aims to identify potential targets within the microglial signaling pathways that could be modulated to mitigate neuroinflammation and restore homeostasis to the brain. This shift in focus not only reinforces the importance of microglial cells in maintaining brain health but also enhances our capacity to develop novel therapeutic strategies that could alter the course of neurodegenerative diseases.
The Future of Alzheimer’s Disease Research
The future of Alzheimer’s disease research is poised for transformative shifts, particularly with the burgeoning understanding of microglial functions and the role they play in disease pathology. As scientists, led by figures like Beth Stevens, delve deeper into the mechanics of microglia and their interactions with neurons, the potential for groundbreaking discoveries increases significantly. The emphasis on holistic approaches, integrating knowledge from immunology, neuroscience, and genetics, is also shaping a new research landscape that prioritizes collaborative efforts and comprehensive investigation of Alzheimer’s mechanisms.
Moreover, as the population ages and the prevalence of Alzheimer’s continues to rise, the urgency for effective interventions becomes increasingly critical. The changing dynamics of research funding and governance are also amplifying efforts to direct funding towards studies aimed at understanding the immunological aspects of Alzheimer’s. With more emphasis on early detection and prevention through novel biomarkers derived from microglial analysis, we may soon witness innovative therapies that change the trajectory of this relentless disease. The integration of technology in research methods also heralds a new era for Alzheimer’s science, with advancements in artificial intelligence and machine learning expected to play a pivotal role in analyzing complex datasets, identifying patterns, and ultimately guiding treatment strategies.
Challenges in Alzheimer’s Disease Therapeutics Development
Despite the promising advances in Alzheimer’s disease research concerning microglial cells and neuroinflammation, the path to developing effective therapeutics remains fraught with challenges. The complexity of Alzheimer’s pathology and the multifaceted role of microglial cells introduce substantial hurdles. Potential therapeutics targeting microglial function must not only mitigate harmful inflammatory responses but should also preserve their protective roles in synaptic maintenance and brain homeostasis. Striking this delicate balance necessitates rigorous preclinical and clinical evaluations, demanding extensive time resources and funding.
Additionally, the variability of Alzheimer’s symptoms and progression among individuals complicates therapeutic development. Treatments that may succeed in one subset of patients may not be effective in another, necessitating a tailored approach that considers genetic, environmental, and lifestyle factors. There is a pressing need for continued investment in research that not only elucidates the fundamental biology of microglial cells but also explores their interaction with other cell types in the brain. Future studies should aim to map the underpinnings of Alzheimer’s complexity to be able to design effective therapies that address root causes rather than just symptoms, ultimately aiming for a cure.
The Intersection of Genetics and Microglial Function in Alzheimer’s
The interaction between genetics and microglial function has emerged as an exciting area of focus in Alzheimer’s disease research. Genetic variants, particularly within genes associated with neuroinflammation, can influence microglial behavior and, consequently, the brain’s immune response. Understanding these genetic underpinnings can provide crucial insights into why certain individuals are at higher risk for developing Alzheimer’s. The APOE4 allele, for instance, has been shown to enhance the inflammatory response of microglia and is one of the most significant genetic risk factors for Alzheimer’s. By studying these genetic markers, researchers are poised to gain a nuanced understanding of how genetic predispositions and microglial dynamics intersect to influence disease onset and progression.
Furthermore, ongoing research into the genetic landscape of Alzheimer’s may lead to discoveries that could inform targeted microglial interventions aimed at modifying disease trajectories. As the field advances, investigations into how specific genetic mutations impact microglial function will be critical in framing personalized treatment plans and identifying at-risk populations. This line of inquiry not only has implications for therapeutic strategies but also underscores the importance of considering genetic and environmental factors equally in the quest to understand Alzheimer’s disease. A comprehensive understanding of these interactions is paramount in paving the way for innovative solutions, potentially leading to breakthroughs that could significantly alter clinical outcomes.
Innovative Technologies in Alzheimer’s Disease Research
The landscape of Alzheimer’s disease research is rapidly evolving, driven by innovative technologies that are redefining how scientists study microglial cells and their role in neurodegenerative processes. Advancements in imaging technologies, such as two-photon microscopy, have enabled researchers to observe microglial behavior in live animal models. This real-time visualization is vital for understanding how microglia interact with neurons during the progression of Alzheimer’s disease. By capturing the dynamics of microglial activity, researchers can gain insights into their dual role in both protecting against and contributing to neurodegeneration, setting the groundwork for developing targeted therapies.
Moreover, the advent of machine learning and artificial intelligence is facilitating the analysis of complex datasets arising from Alzheimer’s research. Large-scale genomic, proteomic, and metabolomic studies are generating voluminous data that can be difficult to interpret. However, machine learning algorithms can help identify patterns and correlations within this data that might elude traditional analysis methods. By applying these technologies, researchers can better understand the multifactorial nature of Alzheimer’s, including the intricate roles that microglial cells play. This intersection of technology and neuroscience promises to unveil novel pathways and correlations, ultimately leading to innovative treatments that can more effectively target the root causes of Alzheimer’s disease.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells are critical to Alzheimer’s disease research as they serve as the brain’s immune system. They patrol for signs of illness and injury, clear damaged cells, and engage in synaptic pruning, which is crucial for healthy neural function. However, dysregulation of microglial activity can lead to excessive pruning, contributing to the neurodegenerative processes seen in Alzheimer’s.
How does synaptic pruning by microglia relate to neurodegenerative disorders like Alzheimer’s?
Synaptic pruning by microglia is a natural process that helps optimize brain connectivity. In Alzheimer’s disease, aberrant microglial pruning can lead to the loss of essential synapses, negatively impacting neuron communication. Research suggests that this malfunction may play a significant role in the progression of neurodegenerative disorders, highlighting the importance of microglial function in maintaining cognitive health.
Are there potential treatments targeting microglia for Alzheimer’s disease?
Yes, recent advancements in Alzheimer’s disease research suggest that targeting microglial cells could lead to novel therapies. By understanding how microglia contribute to neuroinflammation and synaptic pruning, scientists are developing strategies aimed at modulating their activity to prevent or slow the progression of Alzheimer’s and similar neurodegenerative diseases.
What discoveries have been made regarding microglial cells in Alzheimer’s research?
Significant discoveries in Alzheimer’s research have revealed that microglial cells are not merely immune responders, but also play a vital role in shaping neural circuits through synaptic pruning. Aberrant microglial activity has been linked to Alzheimer’s and other neurodegenerative disorders, leading to the exploration of new biomarkers and therapies aimed at correcting these processes.
Why is understanding microglia important in Alzheimer’s disease research?
Understanding microglia is paramount in Alzheimer’s disease research because they are involved in both maintaining brain health and contributing to disease pathology. Their dual role means that insights into microglial function could provide critical information for developing therapeutic interventions to combat neurodegeneration and improve outcomes for individuals with Alzheimer’s.
How do microglial cells influence the brain’s immune system issues in Alzheimer’s?
Microglial cells are the primary immune cells of the brain and play a pivotal role in responding to neuroinflammation, a significant issue in Alzheimer’s disease. When microglial function is compromised, it can lead to heightened inflammation and neuronal damage, exacerbating Alzheimer’s pathology. Therefore, understanding their role can inform strategies for targeting immune-related pathways in treatment.
What impact does NIH funding have on microglial research in Alzheimer’s disease?
NIH funding has been instrumental in advancing microglial research in Alzheimer’s disease. It supports foundational studies that investigate the role of microglial cells in neurodegenerative disorders, enabling scientists like Beth Stevens to explore innovative approaches to treatment and biomarkers that could ultimately improve care for those affected by Alzheimer’s.
How does foundational research on microglia contribute to advances in Alzheimer’s disease understanding?
Foundational research on microglia contributes significantly to our understanding of Alzheimer’s disease by revealing how these cells interact with neurons and participate in synaptic pruning. Such research helps uncover disease mechanisms and may lead to breakthroughs in identifying new therapeutic targets and strategies, ultimately benefiting those with neurodegenerative disorders.
| Key Points | Details |
|---|---|
| Transformation in Understanding Microglia | Beth Stevens’ research has shifted perspectives on microglial cells as crucial immune responders in the brain. |
| Role of Microglia | They patrol for illness, clear dead cells, and prune synapses vital for neuronal communication. |
| Connection to Alzheimer’s Disease | Aberrant pruning by microglia is linked to neurodegenerative diseases like Alzheimer’s and Huntington’s. |
| Importance of Funding | NIH and federal funding have been essential for the foundation and evolution of Stevens’ research. |
| Curiosity-Driven Research | Stevens emphasizes the value of basic science, as it leads to unforeseen discoveries relevant to human health. |
| Impact on Patient Care | Research has potential implications for better detection and treatment options for the 7 million Alzheimer’s patients. |
Summary
Microglia in Alzheimer’s research play a pivotal role in advancing our understanding of neurodegenerative diseases. The groundbreaking work of Beth Stevens has highlighted the dual functionality of microglial cells as both protectors and potential aggressors in brain health. As the research evolves, it not only transforms how we comprehend Alzheimer’s pathology but also opens avenues for innovative biomarkers and therapies to enhance the care for millions affected by this devastating condition.