Medical Research Funding: How Cuts Impact Patient Safety
Medical research funding plays a crucial role in supporting the development of treatments and therapies that enhance patient safety in clinical studies. In recent times, however, significant funding cuts have sparked concerns regarding the integrity of research practices and the ethical oversight necessary to protect participants. The winds of change, particularly those stemming from federal decisions, have hindered the efforts of institutions like Harvard to ensure rigorous IRB oversight, jeopardizing years of collaborative research progress. Without adequate funding, the ability to monitor the rights and welfare of research participants diminishes, causing potential harm and fostering public skepticism. As the landscape of medical research continues to evolve, it is imperative that stakeholders advocate for sustained financial support to uphold the standard of safety that benefits all individuals involved in research.
Financial support for medical studies, often referred to as research financing, serves as the backbone for clinical advancements aimed at improving health outcomes. With recent budget cuts affecting essential grants, the implications for patient care and ethical research practices have raised alarms across the scientific community. As institutions navigate the complexities of these funding challenges, the emphasis on patient security and adherence to institutional review board (IRB) protocols has never been more critical. The ripple effect of diminished resources not only stifles innovation but also undermines collaborative research efforts vital for developing new medical interventions. Ensuring that financial streams remain robust is essential for fostering an environment where the safety of trial participants is prioritized and safeguarded.
The Impact of Funding Cuts on Patient Safety in Medical Research
Funding cuts to medical research present profound challenges, particularly in ensuring patient safety. When financial resources are dwindled, research institutions like Harvard face tough choices that can compromise the rigor of their oversight mechanisms. One of the immediate consequences is the inability of Institutional Review Boards (IRBs) to fulfill their vital roles in safeguarding the rights and welfare of participants. With less funding, IRBs may lack the necessary staffing to thoroughly vet proposals, leaving gaps in compliance with ethical standards and the potential for increased harm to research subjects.
Moreover, these cuts can disrupt the collaborative environment necessary for effective patient safety measures. Many medical studies involve partnerships among hospitals, universities, and regulatory entities, and funding shortages hinder the formation of these critical connections. The SMART IRB system, designed to facilitate multi-site research and ensure consistent oversight, is directly affected by budget constraints, leading to new clinical sites being delayed or added sites not being able to join at all. This halting of collaboration only exacerbates concerns regarding patient safety and the robustness of research protocols.
The Role of NIH Funding in Protecting Patients
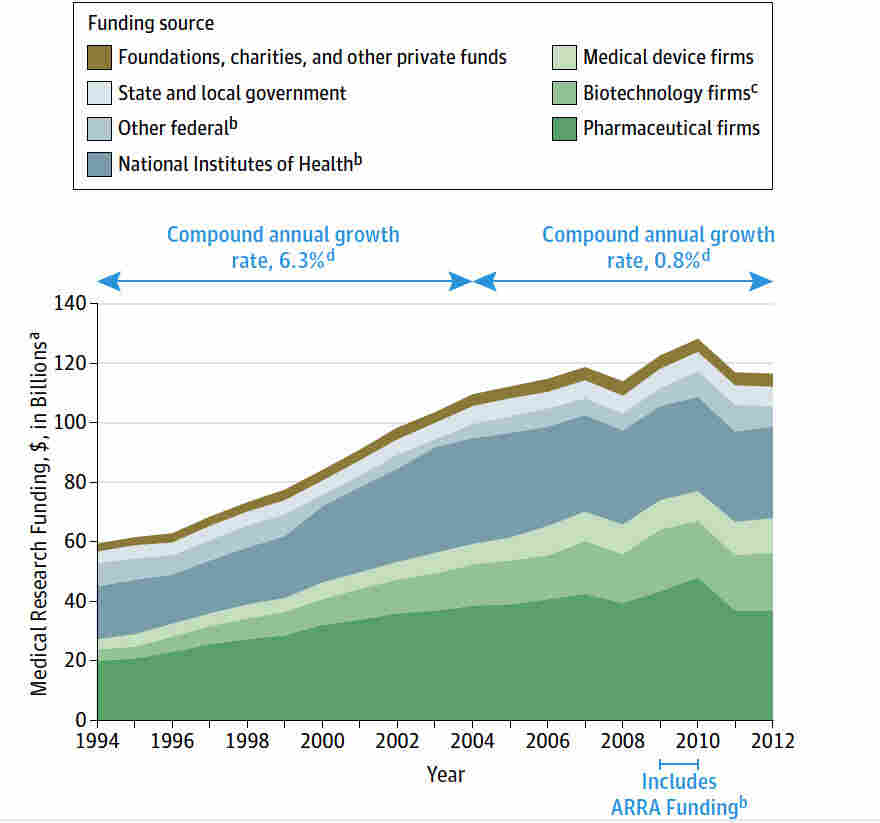
National Institutes of Health (NIH) funding plays a crucial role in the quest to protect patients involved in medical research. By providing financial support specifically targeted at ethical oversight and the health safety of participants, NIH grants enable institutions to maintain rigorous IRB processes. These funds ensure that every research study undergoes extensive scrutiny to align with federal guidelines, thereby fostering a safe clinical research atmosphere. Without sufficient NIH funding, institutions would struggle to uphold their commitment to patient safety, making a strong case for the importance of continued investment in medical research.
Furthermore, NIH funding allows research institutions to implement innovative safety measures and participant safeguards that enhance the reliability of clinical trials. With adequate resources, IRBs can adopt new technologies to improve monitoring and communication with trial participants, thereby enhancing informed consent processes. The strategic infusion of NIH resources cultivates an environment where researchers are not only financially supported in their endeavors but also held to higher standards of ethical conduct – a foundational pillar in ensuring the well-being of patients involved in medical studies.
IRB Oversight: The Backbone of Patient Protection
Institutional Review Boards (IRBs) serve as the backbone of ethical oversight in medical research, ensuring that the rights and safety of participants are paramount. These boards are constituted by varied professionals who meticulously evaluate research proposals for ethical validity and adherence to regulations. Their diverse expertise allows them to assess potential risks, ensuring that participant safety takes precedence through thorough review processes. By keeping patient welfare at the forefront and functioning as a necessary check on research protocols, IRBs represent a critical layer of protection in clinical studies.
Additionally, the involvement of IRBs ensures that research aligns with ethical standards derived from historical lessons in medicine. The establishment of codes and regulations, partly driven by past medical injustices, underscores the need for IRB oversight. The connections between IRBs and federal guidelines reinforce trust in medical research, ensuring participants feel secure in their involvement. However, as funding cuts threaten their operational capabilities, the ability of IRBs to function effectively comes into question, highlighting the urgency of maintaining robust funding for these essential committees.
Collaborative Research: Enhancing Patient Safety Through Cooperation
Collaborative research—the gathering of multiple institutions working together—significantly enhances patient safety and the overall quality of medical studies. This cooperative approach allows for resource sharing, pooling of expertise, and the implementation of best practices that may be more challenging to realize in solitary research endeavors. By working together, institutions can develop a more nuanced understanding of patient needs, better risk assessments, and improved informed consent processes, thereby increasing the overall effectiveness of the research while ensuring patient safety.
However, disruptions in funding undermine these collaborative efforts. When financial support is cut, institutions are often forced to pick and choose projects that can realistically move forward, leading to a decrease in the collaborative networks that can share responsibility for patient safety oversight. This fragmentation weakens the structure of multi-institutional studies that rely on collective wisdom and shared resources, ultimately impacting not just the quality of research but also the safety and experience of patients involved in clinical trials.
The Historical Context of Research Ethics and Patient Safety
Understanding the historical context behind medical research ethics is crucial to appreciating the current frameworks in place that prioritize patient safety. Events such as the Tuskegee Study exposed significant ethical failures, emphasizing the necessity for rigorous oversight systems to protect participant rights. Such historical cases catalyzed the establishment of IRBs, creating a structured environment where ethical considerations are paramount in research proposals. The lessons learned from these past transgressions remain pivotal in the discourse surrounding ethical research conduct.
By reflecting on these historical lessons, modern research has developed into a more ethically aware space, emphasizing informed consent and participant safety. Institutions today, supported by guidelines and funding, strive to ensure that any research conducted is not only scientifically sound but also ethically responsible. This legacy forms the foundation upon which current IRBs operate, ensuring that every participant’s safety is woven into the fabric of the research environment.
Understanding the Consequences of Research Funding Cuts on Public Trust
Funding cuts to medical research can drastically affect public trust in clinical studies. When large-scale grants are halted, and research projects are interrupted, communities may feel anxiety and skepticism about the integrity of research efforts. This erosion of trust can hinder recruitment for future studies, as potential participants might be wary of engaging with research that appears to be underfunded or poorly managed. Indeed, public perceptions of safety can directly correlate with the robustness of research funding, making it essential for institutions to advocate for continued support.
Beyond mistrust from potential participants, funding shortages can also damage the relationship between researchers and the communities they serve. When research efforts fall short of their objectives due to financial constraints, the intended benefits to public health may falter, leading communities to question the motives behind clinical studies. Hence, consistent and reliable funding not only sustains clinical research efforts but also fosters a climate of trust necessary for the continued participation and engagement of the public.
The Intersection of Budget Cuts and Ethical Oversight in Medical Research
Budget cuts pose a distinctive challenge to maintaining ethical oversight in medical research. With diminished resources comes the increased risk of lapses in compliance with ethical standards. Organizations that previously administered comprehensive reviews and supported IRBs may find their capabilities stretched thin, ultimately diminishing patient protections. Financial constraints can lead to less rigorous scrutiny of research proposals, potentially increasing harm to participants, which directly contravenes the principles of ethical research advocacy.
These challenges underscore the necessity for clear communication and advocacy for research funding, as the ethical oversight frameworks need to be upheld in the face of adversity. A concerted effort is required from all stakeholders to recognize that ethical research is not merely a bureaucratic process but a critical aspect of healthcare that translates into real-world patient safety. Measures must be taken to ensure that ethical oversight remains uncompromised amid budget cuts, advocating for creative solutions that can continue to protect patient interests in the research arena.
The Future of Medical Research in an Era of Funding Shortages
The future of medical research is gravely contingent upon sustaining funding levels amidst increasing competition for grants and financial support. The recent cuts have illuminated the fragility of funding, raising concerns about the long-term viability of groundbreaking studies that prioritize patient safety. Researchers and institutions alike must proactively advocate for increased federal support, particularly from entities like the NIH, which play a critical role in fueling innovation and ethical research practices.
Moving forward, it is imperative for the research community to foster collaborations that leverage shared resources and emphasize patient safety. By cultivating partnerships to address funding shortages, researchers can innovate within restrictive budgets while maintaining high ethical standards. Community engagement and transparency will also be key components in restoring trust, ensuring that participants remain at the forefront of the research agenda despite the challenges posed by funding cuts.
Frequently Asked Questions
What is the impact of funding cuts on patient safety in medical research?
Funding cuts, such as those experienced by institutions like Harvard, lead to disrupted systems like SMART IRB that ensure patient safety in medical research. Without adequate resources, oversight mechanisms can weaken, jeopardizing the rights and welfare of participants involved in research studies.
How does NIH funding contribute to patient protection in medical research?
NIH funding plays a critical role in protecting patients in medical research by supporting institutional review boards (IRBs) that oversee studies involving human participants. These funds help ensure that research complies with ethical standards and regulations aimed at safeguarding participant welfare.
What is the role of IRB oversight in safeguarding patients during medical research?
IRB oversight is essential in medical research, as it involves reviewing and approving study protocols to protect participants. By assessing risks, ensuring informed consent, and monitoring adverse events, IRBs help maintain ethical standards and prioritize patient safety in research initiatives.
How do collaborative research efforts benefit from NIH funding?
NIH funding facilitates collaborative research by providing support for single IRBs (sIRBs), which streamline the review process for multisite studies. This collaboration reduces the administrative burden on researchers and enhances the efficiency of conducting studies that ultimately improve patient care.
In what ways do funding cuts affect institutions’ ability to conduct medical research safely?
Funding cuts can halt ongoing research, leading to delays and preventing institutions from adding new clinical sites. This disruption undermines the ethical oversight provided by IRBs, potentially exposing participants to unmonitored risks, which ultimately threatens patient safety and public trust in research.
What are the consequences of interrupted IRB processes due to funding issues?
Interrupted IRB processes caused by funding issues can risk causing harm to participants as studies may halt midstream. This can also foster public skepticism and diminish institutional commitment to ethical research practices, making it challenging to maintain patient safety in medical research.
| Key Points | Details |
|---|---|
| Impact of Funding Cuts | Funding cuts have disrupted crucial patient safety measures in medical research and hindered oversight. |
| SMART IRB Overview | The SMART IRB is an institutional review board system that ensures patient protection across multiple research sites. |
| Role of IRBs | IRBs review research proposals, ensuring compliance with ethical standards and participant safety. |
| Historical Context | Past unethical research practices have led to the establishment of stringent IRB oversight to protect participants. |
| Consequences of Halting Research | Halted studies can lead to long-term harm and erode public trust in medical research. |
| Continued Support | Despite funding cuts, Harvard Medical School is providing support to maintain essential research oversight. |
Summary
Medical research funding is vital for ensuring the safety of patients involved in clinical studies. The recent freeze of over $2 billion in federal research grants at Harvard has severely disrupted patient protection efforts. With oversight mechanisms like the SMART IRB facing operational halts, the integrity of medical studies is at risk, leading to potential harm to patients and diminished public trust in medical research. This situation underscores the critical importance of sustained funding in the realm of medical research to uphold ethical standards and patient safety.