Pediatric Brain Cancer Relapse Prediction Using AI Tools
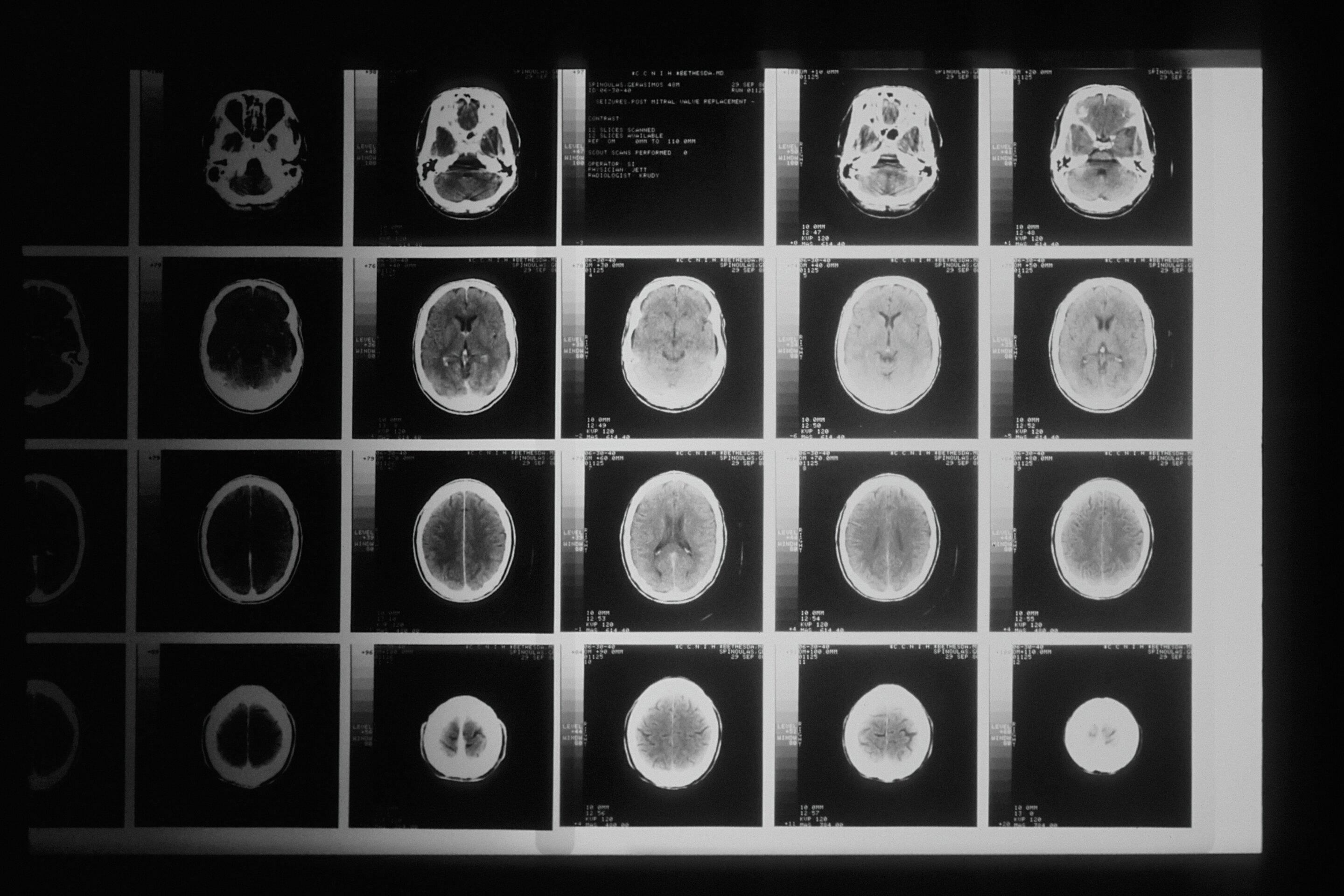
Pediatric brain cancer relapse prediction is an urgent area of research that has gained momentum thanks to advancements in artificial intelligence. Recent studies indicate that AI tools, especially those utilizing machine learning in medicine, significantly enhance the accuracy of predicting recurrence in children with brain tumors, such as gliomas. By analyzing multiple imaging scans over time, these innovative technologies can offer insights far surpassing traditional methods, paving the way for improved patient outcomes. As glioma treatment advancements progress, clinicians are increasingly able to identify at-risk patients early, thus alleviating the stress of frequent MRIs for families. This research underscores the potential of brain cancer imaging technology in revolutionizing how pediatric oncology addresses cancer recurrence, ensuring that children receive tailored, effective care.
The prediction of relapse in childhood brain tumors represents a vital intersection of technology and medicine, where innovative strategies are essential for enhancing patient care. As pediatric cancers become more treatable, the focus on detecting early signs of recurrence is paramount. Advanced imaging techniques, in conjunction with data-driven approaches, empower healthcare professionals to identify high-risk patients and optimize treatment plans. The transformative role of artificial intelligence in this field not only streamlines the diagnostic process but also seeks to mitigate emotional and logistical burdens faced by families. By leveraging machine learning, the landscape of pediatric brain cancer management is evolving, aiming for better prognostic tools that prioritize the well-being of young patients.
AI in Pediatric Oncology: A Game Changer for Relapse Predictions
Artificial Intelligence (AI) is revolutionizing the landscape of pediatric oncology by providing enhanced predictive tools that help doctors anticipate cancer relapses in children. Traditional methods for predicting pediatric brain cancer relapse often rely on singular imaging and clinical assessments, which can lack the nuance needed to foresee recurrence effectively. In a study conducted by researchers from Mass General Brigham, an advanced AI model demonstrated significant improvements in predicting the risks associated with pediatric gliomas, outperforming conventional techniques. This innovation allows for more tailored and potentially less invasive follow-up care for young patients.
The application of AI in pediatric oncology goes beyond mere prediction; it offers a transformative approach to managing patient care. With the ability to analyze extensive datasets, including thousands of brain scans, AI tools can detect subtle changes over time that may signal a return of cancer. This predictive capability ultimately aims to alleviate the burden of continuous imaging for families and children, providing peace of mind while enabling healthcare providers to identify those at the highest risk more quickly. As researchers continue to refine these AI techniques, the potential for application in various cancer settings becomes increasingly promising.
Glioma Treatment Advancements Through Machine Learning
Recent advancements in glioma treatment are being propelled by breakthroughs in machine learning technologies. These systems can process large volumes of imaging data, identifying complex patterns that traditional methods might overlook. The research from Mass General Brigham highlighted the use of temporal learning, which analyzes a series of scans rather than relying on a snapshot. This innovative approach allows for better-informed decisions regarding treatment plans and follow-up care, providing oncologists with a more detailed understanding of a patient’s condition over time.
Machine learning models are particularly beneficial in managing pediatric gliomas, as they can adjust to individual patient histories and provide nuanced treatment options based on previous responses to therapy. By integrating these models into pediatric oncology practices, healthcare providers can work towards personalized treatment strategies that adapt as patients progress through their treatment journeys. The hope is that such advancements can help lower recurrence rates and improve overall outcomes for children afflicted with this challenging form of cancer.
The Future of Brain Cancer Imaging Technology
The future of brain cancer imaging technology is bright, thanks in large part to advancements in AI and machine learning. Innovations in imaging techniques will allow healthcare providers to monitor brain tumors in real-time, offering deeper insights into the progression of diseases like gliomas. The research demonstrated how AI can learn from multiple imaging sessions, utilizing data from upto 4,000 MRI scans to accurately predict cancer recurrence within a year post-treatment. This capability represents a significant shift in how pediatric brain tumors may be approached in the future.
Moreover, as imaging technology continues to evolve, it is expected to integrate seamlessly with treatment protocols, allowing for adaptive therapies. This could include fine-tuning treatment plans based on AI insights and reducing the frequency of imaging for low-risk patients while increasing focus on those who are at a greater risk of recurrence. Such advancements not only enhance survival rates but also improve the overall quality of life for young patients and their families. The potential for these technologies to aid in the early identification of issues will undoubtedly reshape the standard of care in pediatric oncology.
Predicting Cancer Recurrence: An Urgent Need in Pediatric Oncology
Predicting cancer recurrence is an urgent need in pediatric oncology, especially for conditions like gliomas. Children who undergo treatment for brain tumors often face the possibility of relapse, making it essential to have reliable methods for forecasting their prognosis. The traditional methods, which often depend on infrequent imaging and clinical evaluation, can be insufficient. The implementation of AI-driven algorithms signifies a crucial advancement in overcoming these challenges, providing timely and accurate predictions that allow for proactive patient management.
As the field of pediatric oncology evolves, the ability to predict cancer recurrence with greater accuracy will transform care standards. With the pressure on healthcare providers to deliver personalized medicine, the creation of robust predictive models will enhance decision-making for oncologists. This is critical not only in reducing the stress on patients and families but also in ensuring that treatment strategies are appropriately scaled to the individual patient’s risk profile, potentially leading to more favorable outcomes.
Machine Learning in Medicine: Transforming Pediatric Tumor Care
The rise of machine learning in medicine is transforming the landscape of pediatric tumor care, particularly with brain cancers. Machine learning algorithms can process immense amounts of data, allowing healthcare professionals to glean insights that would otherwise remain hidden. Through the synthesis of longitudinal imaging data, machine learning models can unveil patterns of tumor growth and behavior over time, enabling accurate predictions regarding the likelihood of relapse.
In the context of pediatric oncology, this means that treatments can be better aligned with each patient’s unique tumor profile. For tumors like gliomas, the ability to integrate data from multiple sources into a coherent predictive model enables physicians to adopt more informed and targeted approaches to care. Thus, as machine learning continues to develop, its application in predicting outcomes for young cancer patients offers hope for more effective, less invasive treatment strategies tailored specifically for children.
The Role of AI in Enhancing Pediatric Brain Tumor Outcomes
AI is poised to play a crucial role in enhancing outcomes for children with brain tumors. By employing data-driven technologies, healthcare providers can shift from reactive to proactive approaches in managing pediatric brain cancer. The AI model developed in the Mass General Brigham study demonstrated accuracy that far surpassed traditional predictive techniques, promising improvements in how oncologists monitor and treat pediatric patients at risk for glioma recurrence.
With ongoing research, the integration of AI into clinical practice could lead to the development of new standards for follow-up care in pediatric oncology. AI-tuned strategies may help reduce unnecessary interventions for low-risk patients while simultaneously ensuring that those high-risk patients receive the necessary aggressive treatments. This dual approach optimizes care by focusing resources effectively where they are needed most, showcasing how innovative technology can enhance survival rates and reduce cancer burdens.
Key Challenges in Implementing AI for Pediatric Brain Cancer
Despite the promising advances AI presents to pediatric oncology, key challenges remain in effectively implementing these technologies. Data privacy, the necessity for high-quality datasets, and ensuring that AI systems are unbiased are significant hurdles to overcome. As AI continues to be integrated into clinical settings, it is critical for researchers and healthcare providers to address these concerns diligently to foster trust and acceptance among patients and professionals alike.
Furthermore, the clinical validation of AI models must be rigorously tested across diverse populations to ensure the algorithms are generalizable and effective. Ongoing collaboration between researchers, technologists, and clinicians will be necessary to refine these tools and facilitate their adoption into standard care protocols. Only through addressing these challenges can the full potential of AI in pediatric brain cancer care be realized.
Future Directions in Pediatric Oncology Research
Future directions in pediatric oncology research are increasingly focused on leveraging AI and machine learning technologies to improve patient outcomes. With the ongoing exploration of AI’s capabilities, researchers are optimistic about developing enhanced predictive tools for tumor management. By combining clinical expertise with advanced imaging technology, teams can gain a comprehensive understanding of tumor biology, paving the way for precision medication tailored to the unique needs of pediatric patients dealing with gliomas.
Moreover, as the field expands, it is expected that research will delve into integrating genetic information with imaging data, creating a multifaceted approach to predicting recurrence risks. This comprehensive strategy can ultimately lead to the development of targeted therapies that enhance treatment efficacy while minimizing adverse effects. As these insights are uncovered, the hope is to refine and improve care pathways to ensure the best possible outcomes for children battling brain cancer.
Integrating Family Support in Pediatric Brain Cancer Treatment
Integrating family support into pediatric brain cancer treatment is crucial for enhancing the overall care experience for young patients. Families play an essential role in the treatment process, providing emotional and logistical support as their child undergoes difficult therapies. By ensuring that families are involved in care decisions and informed about treatment plans, healthcare providers can create a supportive environment that addresses the emotional and psychological needs of both patients and their families.
Furthermore, education about the predictive models being utilized, such as those involving AI, can empower families, allowing them to engage actively with healthcare providers. This collaboration can assist in alleviating anxiety surrounding treatment and recurrence risks. As the field of pediatric oncology evolves, fostering strong family support systems will be fundamental in ensuring holistic care and improving outcomes for children affected by brain tumors.
Frequently Asked Questions
What is the role of AI in pediatric brain cancer relapse prediction?
AI plays a crucial role in pediatric brain cancer relapse prediction by analyzing multiple brain scans over time to identify subtle changes that indicate a risk of cancer recurrence. This advancement allows for more accurate predictions than traditional methods, ultimately enhancing patient care and outcomes.
How does machine learning improve predicting cancer recurrence in children?
Machine learning improves predicting cancer recurrence in children by leveraging vast amounts of medical imaging data. In pediatric brain cancer, especially gliomas, AI models trained with temporal learning can synthesize information from multiple MR scans to detect patterns that signal a higher likelihood of relapse, leading to timely interventions.
What are glioma treatment advancements associated with AI technologies?
Glioma treatment advancements using AI technologies include improved accuracy in predicting relapse, personalized treatment plans based on risk assessments, and potentially reducing the frequency of follow-up imaging, which can ease the burden on patients and families. These advancements rely on sophisticated algorithms that analyze serial imaging data.
Can brain cancer imaging technology aid in predicting pediatric cancer recurrence?
Yes, brain cancer imaging technology significantly aids in predicting pediatric cancer recurrence by providing detailed MR scans that AI algorithms analyze over time. This comprehensive approach enhances the understanding of tumor behavior post-treatment, ultimately improving relapse prediction accuracy.
What is temporal learning, and how does it impact pediatric brain cancer relapse prediction?
Temporal learning is a machine learning technique that utilizes sequences of brain scans taken over time. In pediatric brain cancer relapse prediction, this method allows AI models to recognize changes associated with tumor recurrence by understanding how tumors develop and respond to treatment, leading to more reliable risk assessments.
What are the potential benefits of using AI for predicting pediatric glioma recurrence?
The potential benefits of using AI for predicting pediatric glioma recurrence include increased accuracy in identifying at-risk patients, the ability to tailor follow-up care based on individual risk levels, and the possibility of optimizing treatment strategies, which can lead to better patient outcomes and reduced psychosocial stress for families.
How accurate are AI methods in predicting pediatric brain cancer relapse compared to traditional methods?
AI methods, particularly those employing temporal learning, have shown predictive accuracies of 75-89% for pediatric brain cancer relapse, significantly outperforming traditional methods, which only achieved about 50% accuracy. This highlights the transformative potential of AI in improving clinical decision-making.
Will AI-informed risk predictions reduce the stress of follow-up imaging for pediatric glioma patients?
Yes, AI-informed risk predictions are anticipated to reduce the stress of follow-up imaging for pediatric glioma patients by allowing healthcare providers to identify low-risk patients who may require less frequent imaging. This targeted approach can alleviate unnecessary anxiety for children and their families.
What future developments are expected in pediatric brain cancer relapse prediction using AI?
Future developments in pediatric brain cancer relapse prediction using AI include further validation of temporal learning techniques in clinical settings, the initiation of clinical trials to test AI-informed strategies, and potential integration of AI models into routine care to enhance early identification of high-risk patients.
| Key Points | Details |
|---|---|
| Study Overview | AI tool surpasses traditional methods in predicting pediatric brain cancer relapse. |
| Purpose | Improve identification of children at risk of brain tumor recurrence, specifically gliomas. |
| Methodology | Nearly 4,000 MRI scans from 715 pediatric patients used, with a focus on multiple scans over time for better prediction. |
| Temporal Learning | Innovative technique allowing the AI to analyze changes across multiple images instead of single scans, leading to improved accuracy. |
| Accuracy | 75-89% accuracy in predicting recurrence, significantly higher than 50% accuracy from single image predictions. |
| Future Steps | Plans to validate the AI model further and potentially launch clinical trials to enhance patient care strategies. |
Summary
Pediatric brain cancer relapse prediction is a critical area that has been notably improved through recent advancements in AI technology. The innovative study highlights how an AI tool can analyze a series of MRI scans over time, thus providing more accurate predictions of relapse risk in pediatric glioma patients compared to traditional single-scan methods. As researchers continue to refine these AI models and validate their effectiveness, there is an optimistic prospect for enhanced pre-treatment strategies that can lead to better outcomes for children facing brain cancer.